Did you know that medical practices, including home health providers, lose up to 25% of their income because of unpaid claims?
Focus More on Patient Care
With the stress of paperwork and payments entrusted in the hands of a billing service, you will be free to redirect your attention to offering quality care to your patients. This will bring them the utmost satisfaction which will lead to more credibility for your agency, and increase patient flow, eventually generating more
revenue.
Customizable Plans
With no sign-up fees, we cater and customize our services to meet your specific requirements. Our goal is to simplify your billing procedures while increasing efficiency and accuracy to enhance revenue and reduce billing loss.
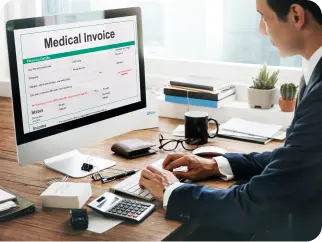
Improve Accuracy
Medical billing errors are a major problem in the US healthcare system. According to studies, over 80% of medical bills contain inaccuracies. Using a medical billing service can help prevent revenue loss or delay by checking all claims before submitting them.
Why People Trust Us
We assist healthcare professionals, practices, and organizations in managing the financial aspects of patient care efficiently.

Insurance Eligibility Verification
Patient insurance eligibility is verified prior to all billing to ensure that healthcare providers will be paid for the services they render. It helps prevent claim denials and rejections, which can result in financial losses.

Claim Submission
Claims and corrections are submitted within 24-48 hrs of notice. Prior to claim submission, we check for completeness and compliance of patient charts. We strive for a clean claim rate of 99% for faster reimbursement and fewer denials/rejections.
Follow-Up
With our A/R management team, we monitor all aged claims and take immediate action on untimely reimbursements. All claim follow-ups get recorded and shared with you.

Payment Posting
Payer remittances and EOBs are managed on a daily basis. Each payment is verified to ensure claims are paid appropriately. Denied and reduced claims are forwarded to our A/R department.
Denials and Appeals
Claim denials and appeals are handled within the Timely Filing Limits of each payer. Our aim is to have claims paid after the first round of re-processing or first level of appeal.
Data and reporting
Get valuable insights with customizable reports based on your preferences. These insights offer a clear understanding of any trends and your organization’s performance by revealing patterns and tracking progress. Reports can help organizations identify strengths and weaknesses making data-driven improvements easier.
Questions regarding our services?
Schedule a free consultation with NO obligations
Our Services
Testimonials
What Our Clients Say
Related Articles and News
Be the first to read
Related Articles and News
Be the first to read
Avara MedSolutions
Top medical billing service providers based in
California
Have a Question? Ask Us.
Have a Question? Ask Us.
Medical Billing Starting At 1%
Book An Appointment
Avara MedSolutions offers revenue cycle management for healthcare organizations. We maximize collections, improve cash flow, and ensure compliance with quick turnaround times. Contact us for reliable and valuable services.
Cum sociis natoque penatibus et magnis dis parturient ntesmus. Proin vel nibh et elit mollis commodo et nec augue tristique sed Quisque velit nisi, pretium ut lacinia lementum id enim. Nulla quis lorem ut libero malesuada feugiat.
Cum sociis natoque penatibus et magnis dis parturient ntesmus. Proin vel nibh et elit mollis commodo et nec augue tristique sed Quisque velit nisi, pretium ut lacinia lementum id enim. Nulla quis lorem ut libero malesuada feugiat.
Cum sociis natoque penatibus et magnis dis parturient ntesmus. Proin vel nibh et elit mollis commodo et nec augue tristique sed Quisque velit nisi, pretium ut lacinia lementum id enim. Nulla quis lorem ut libero malesuada feugiat.
Cum sociis natoque penatibus et magnis dis parturient ntesmus. Proin vel nibh et elit mollis commodo et nec augue tristique sed Quisque velit nisi, pretium ut lacinia lementum id enim. Nulla quis lorem ut libero malesuada feugiat.